Elements from the patient history that raise suspicion of SBO include history of previous abdominal surgery, absence of flatus and bowel movements, nausea, and pain relieved by vomiting.3 Abnormal bowel sounds, abdominal distension, tympany to percussion, and tenderness are important findings on the physical exam.3 High-pitched bowel sounds may be auscultated in early obstruction in comparison to minimal bowel sounds heard as the bowels become hypotonic in later SBO.3 Common causes of bowel obstruction include adhesions, neoplasms, herniation, and inflammatory bowel disease.3 The most common cause of SBO is adhesions subsequent to lower abdominal surgeries such as appendectomies, colorectal surgery, and hernia repairs.3
The history and physical exam alone are insufficient to diagnose SBO and diagnostic imaging is required.1 Diagnostic tests available include plain radiographs, ultrasonography (US), computed tomography (CT), and magnetic resonance imaging (MRI).
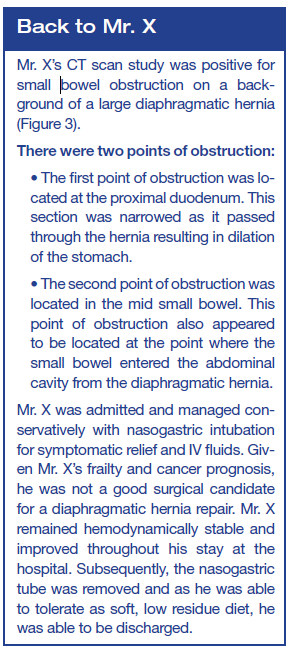
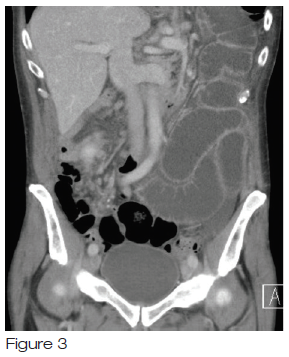
(CT), magnetic resonance imaging (MRI), and ultrasound have all been shown to be effective at making the diagnosis of SBO, with plain radiography being non-diagnostic and non-specific in many cases4 (sensitivity 59%, specificity 77%).2 However, plain films remain part of the initial evaluation due to their availability, low cost, and ability to follow disease progression. 4 The “gold standard” for the diagnosis of SBO is CT (with or without intravenous contrast).1,6 CT scans (abdomen and pelvis) should be considered in all patients with SBO in order to provide important information on etiology, severity, and management of SBO.
a transition point, where proximal bowel is dilated and distal bowel is decompressed,
decompressed colon,
inability of contrast to pass transition point
Point of Care Ultrasound (PoCUS) is an alternative to x-ray and CT to detect SBO. PoCUS, a very accurate test and useful for rapid detection of SBO, is performed with a curvilinear low-frequency probe, and is easy to learn1,6 (sensitivity 93-100%, specificity 81.4%-100%.).5> Criteria for PoCUS SBO diagnosis include >2.5cm dilated loops of bowel, abnormal peristalsis activity, and resulting in stasis or to-and-fro motion of bowel contents.6 Another clinical sign of SBO is the “keyboard sign”, where the plicae circulares become apparent as finger-like projections from the inner wall of the intestine, a surrogate for wall edema.7
Bedside ultrasound has the potential to expedite diagnosis of and/or exclude SBO in the emergency department allowing for the prompt initiation of treatment with nasogastric suction.1 However, PoCuS fails to provide the clarity of a CT in revealing the cause of the SBO.
Early management of SBO involves nasogastric tube decompression, intravenous fluid resuscitation guided by urine output.3 For clinically stable patients with partial or complete obstruction, conservative management as previously described is recommended. If there are no signs of improvement/resolution after 48 hours, a water-soluble contrast study or surgery is indicated.3 Surgical treatment may be required if the patient is not clinically stable suggesting perforation or vascular compromise which will be identified on CT.3,4
References
Carpenter CR, Pine JM. The End of X-rays for suspected Small Bowel Obstruction? Using Evidence-based Diagnostics to inform Best Practices in Emergency Medicine. Acad Emerg Med 2013; 20(6):618-20
Guttman J, Stone MB, Kimberley HH, et al. Point-of-Care ultrasonography for the diagnosis of small bowel obstruction in the emergency department. CJEM 2015; 17(2);206-9.
Jackson PG, Raiji M. Evaluation and Management of Intestinal Obstruction. Am Fam Physician 2011; 83(2):159-65
Maung AA, Johnson DC, Piper GL, et al. Evaluation and management of small-bowel obstruction: An Eastern Association for the Surgery of Trauma practice management guideline. J Trauma Acute Care Surg 2012; 73(5):S362-9
Pourmand A, Dimbil U, Drake A, et al. The Accuracy of Point-of- Care Ultrasound in Detecting Small Bowel Obstruction in Emergency Department. Emerg Med Int 2018; 1-5. ID 3684081.
Taylor MR, Lalani N. Adult Small Bowel Obstruction. Acad Emerg Med 2013; 20(6):529-44
Taylor T, Meer J, Beck S. Emergency Ultrasound: Bedside Ultrasound to Diagnose Small Bowel Obstruction. Emerg Med 2014; 46(8):369-70